The retina is responsible for creating the images that we see and functions very similar to the film at the back of a camera. The central part of the retina is called the macula. It has the highest density of light detecting cells known as photoreceptors and is responsible for detailed vision required in activities such as reading and recognising faces. When the retina separates from the back wall of the eye, it is detached from its blood supply and nutrition source. If a detachment of the retina is left untreated, the macula is likely to become involved in the retinal detachment resulting in loss of central vision. Further delay in treatment will result in irreversible visual loss.
There are three different types of retinal detachment:
1) Rhegmatogenous Retinal Detachment
A rhegmatogenous retinal detachment is the most common type of retinal detachment and it occurs because there is a retinal tear or a hole in the retina. This tear in the retina can occur when the vitreous separates from the surface of the retina during a process known as a posterior vitreous detachment or a PVD.
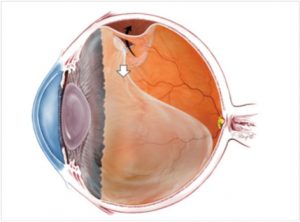
The Symptoms of a PVD include flashes and floaters that appear as curly lines and dark spots that move with your eye. Not all posterior vitreous detachments will cause a tear in the retina. However, if a tear in the retina occurs from the posterior vitreous detachment, then fluid from the vitreous cavity can seep under the retina through the tear to detach the retina. This is demonstrated in figure 1.
Figure 1: The vitreous is like a balloon filled with jelly (vitreous gel) that fills the back chamber of the eye. The skin of this balloon of jelly at some time in life from the age of about 40 will separate from the retinal surface as shown in the diagram below (Posterior vitreous detachment or PVD). In areas where the vitreous is more firmly attached to the retinal surface, usually in the peripheral retina, a flap of retina can be pulled of by the vitreous, resulting in a retinal tear. With time, fluid from the vitreous cavity can migrate into the potential space under the retina through this tear to cause a retinal detachment. Note: the diagram shows an early retinal detachment which can progress over time.
If a retinal tear is detected early at the time of a PVD, it can be treated with either retinal laser (laser retinopexy) or freezing (cryotherapy). Both treatments result in the formation of a stable scar around the retinal tear that seals off the tear preventing vitreous cavity fluid from detaching the retina. Thus, early detection and treatment of a retinal tear with either laser or cryotherapy reduces the risk of this progressing to become a retinal detachment.
Most retinal detachments begin first in the peripheral retina, which manifests as a shadow creeping in from one’s peripheral field of vision. As the detachment extends to involve the macula or central retina, central vision will be lost. Once the retina is detached, surgery is necessary to recover some of the vision that is lost and also to prevent further visual loss. The amount of vision that can be recovered from successful retinal detachment surgery is variable and depends largely on how well the eye heals itself once the retina is put back into its correct anatomical position by surgery. Ideally, retinal detachment surgery is performed before the central retina or macula is involved in the detachment, allowing for the preservation of central vision, hence the importance of early presentation to your eye doctor whenever you have symptoms of a posterior vitreous detachment or a retinal detachment. These symptoms are the perception of flashing lights in one’s visual fields particularly in dim lighting conditions and black dots or flecks floating around like small insects in one’s field of vision. Surgery is successful in reattaching the retina in up to 90% of cases.
There are several surgical procedures that can be used to repair a retinal detachment.
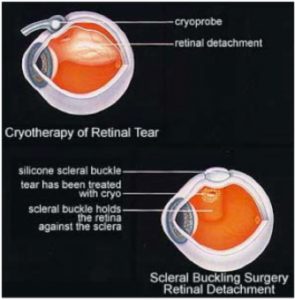
1) Scleral Buckle
In this procedure, the skin or conjunctiva of the eye is carefully dissected from the surface of the eye and a synthetic band often made from silicone is sewn on to the external coat of the eye called the sclera. Fluid under the retina can be drained with a needle passed into the space under the retina created by the detachment (subretinal space) through the scleral wall and the retinal tear is treated with freezing or cryotherapy. The scleral buckle reduces the amount of fluid that recruits into the subretinal space through the tear.
Figure 2: Scleral buckle for retinal detachment repair
2) Vitrectomy
Vitrectomy surgery has been used in the treatment of retinal detachments for over 35 years. By making 3 small keyhole incisions into the eyeball, instruments are able to be inserted into the middle of the eyeball to remove the bulk of the vitreous gel. This is necessary to relieve the traction of the vitreous on the retinal tears and also to create a space whereby a gas bubble can be injected into the eye to displace the fluid from under the retina and splint the retina into place.
Figure 3: Schematic diagram showing a vitrectomy being performed to remove the vitreous gel.
About 90% of rhegmatogenous detachments can be repaired initially with either one or both procedures.
Following retinal detachment surgery, the eye may feel uncomfortable and appear red and injected for several weeks during the postoperative healing process. It is not unusual for the eye to feel gritty and watery. If severe pain persists or there is discharge from the eye, it is important for you to contact your surgeon so that severe problems such as infection can be ruled out. The vision may take months to recover but usually patients notice a significant improvement in their vision once the gas bubble used to support the retina, goes away completely. As the gas bubble resorbs spontaneously, the eye will replenish this volume with a saline like solution called the aqueous. The level between the gas and the aqueous is called a gas – fluid level and it will feel like you are walking around with a spirit level in your eye. While there is gas in the eye, you may be instructed by your surgeon to posture in a particular position. You will not be able to drive a car with gas in the eye, up to several weeks following retinal detachment surgery. If there is gas in the eye, you will also not be able to fly in a plane as the gas will expand in a confined space at altitude, causing the pressure within the eye to rise to a dangerous level resulting in permanent irreversible complete loss of vision.
2) Exudative Retinal Detachment
Exudative retinal detachment occurs when fluid leaks into the space under the retina due to inflammatory conditions, tumors of the choroid, or due to an unknown cause. Exudative retinal detachments are not caused by a tear in the retina and as such, the treatment of exudative retinal detachment does not usually involve surgery, but more targeted towards the underlying cause. Non invasive investigations that may help illucidate the underlying cause such as an ultrasound of the choroid, an angiogram looking at the retinal and choroidal circulation and a retinal OCT scan may need to be performed.
3) Traction Retinal Detachment
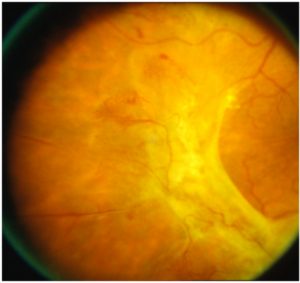
A tractional retinal detachment occurs when fibro-vascular tissue within the vitreous cavity pulls on the retina eventually causing it to detach. The most common cause of a tractional retinal detachment is the late stages of proliferative diabetic retinopathy. Tractional retinal detachments involving the peripheral retina may be observed, but if the macula is involved in the tractional detachment, then surgery is usually indicated to relieve the traction on the retina.
Figure 4: Retinal photograph showing fibrovascular tissue proliferating on the surface of the retina causing a tractional retinal detachment.