Diabetes is a cause of severe visual loss and blindness due to its effects on the circulation of the retina. Damage to the small blood vessels that supply blood to the retina (the retinal capillaries) causes visible changes to the retina such as bleeding or cholesterol deposition within the retina. These visible signs of damage to the retina due to diabetes are collectively known as diabetic retinopathy. Poor control of blood sugar levels, blood pressure and cholesterol levels are known factors which accelerate the worsening of diabetic retinopathy. The longer someone has diabetes, the more likely they are also to have diabetic retinopathy.
Often, loss of vision from diabetic retinopathy is not evident to the patient until it is advanced and as such retinal examinations by a clinician at regular intervals are recommended and essential to detect damage to the retina at a time when treatment can be started to prevent the vision from becoming worse and in some cases even to improve vision.
Types of Diabetic Retinopathy
1) Diabetic Maculopathy – Diabetic retinal damage to the Macula (Central retina)
Diabetes can cause the capillaries (small blood vessels) supplying blood to the macula to become leaky thus causing the retina to become swollen (edematous) resulting in loss of central vision. This is known as Diabetic Macular Edema (DME). Conversely, diabetes can also cause the capillaries to become blocked off hence causing the macula to be starved of nutrients, again causing loss of central vision. This is known as Macular Ischaemia.
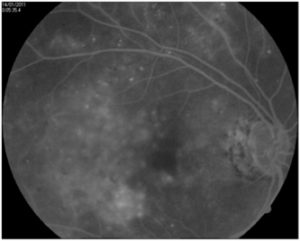
A fluorescein angiogram which is a test involving the injection of dye into the venous circulation followed by retinal photography to study the retinal circulation is often performed when DME or macular ischaemia is present as this helps guide treatment (see section on Fluorescein Angiogram). An Optical Coherence Tomography (OCT) scan which shows the retina in magnified cross section will also be performed to assess the degree of retinal swelling/edema present.
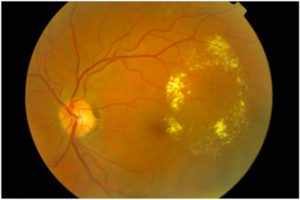
Figure 1: Photo of the retina showing diabetic macular edema with leakage from the microaneurysms (red dots) and deposition of cholesterol visible as yellow flecks into the retina.
Figure 2: A fluorescein angiogram demonstrating the leakage of fluorescein dye into the retina due to the leaky capillaries in a patient with severe diabetic macular oedema
Figure 3: An OCT scan showing the retina in magnified cross section. The cystic fluid filled spaces is the edematous fluid accumulating within the retina in diabetic macular oedema.
2) Non Proliferative Diabetic Retinopathy (NPDR)
Damage to the retinal capillaries supplying the peripheral retina is visible on examination of the retina as retinal haemorrhages, microaneurysms and infarctions of the nerve fibre layer of the retina. These signs on examination of the retina are known collectively as Non Proliferative Diabetic Retinopathy (NPDR). Usually at this stage of the disease, the patient is not symptomatic of any change in vision.
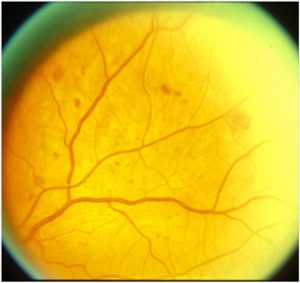
Figure 4: Color photo of the retina showing the retinal haemorrhages in non proliferative diabetic retinopathy. Often at this stage even when there is visible damage to the retina from longstanding diabetes, the patient is unaware of any changes in their vision.
3) Proliferative Diabetic Retinopathy (PDR)
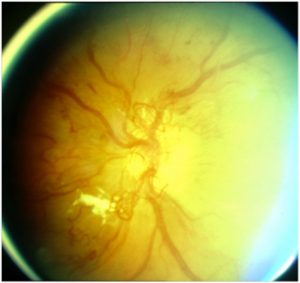
Non proliferative diabetic retinopathy can progress over time to the next stage of the disease process called proliferative diabetic retinopathy. During this stage, abnormal fragile blood vessels start to grow on the surface of the retina. These blood vessels are likely to bleed over time into the vitreous cavity (vitreous haemorrhage) resulting in visual loss. These abnormal blood vessels can also become scar tissue that pulls on the retina causing it to become detached from the surface of the retina (tractional retinal detachment).
Figure 5: Abnormal blood vessels are visible on the optic disc whereby non proliferative diabetic retinopathy (NPDR) has now progressed to proliferative diabetic retinopathy (PDR)
Figure 6: Bleeding from the abnormal blood vessels in proliferative diabetic retinopathy (PDR) visible as a crescent shaped layer of blood deposited on the surface of the retina.
Treatment Options
Modification of systemic parameters
Tight control of blood sugar levels, blood pressure and lipid levels is very important in slowing the progression of diabetic retinopathy and also reducing the risk of visual loss
1) Treatment for Diabetic Macular Edema
a) Macular laser for diabetic macular oedema
Once diabetic macular oedema has progressed to a certain stage, retinal laser may be necessary. Because the laser is applied to the macula where the retinal swelling is, this procedure is called macular laser. Macular laser is performed in the clinic rooms. During the procedure, laser light is delivered to the retina through a dilated pupil via a hand held contact lens which is placed on the surface of the eye following the application of local anaesthetic to the eye to numb the surface of the eye. Patients are advised not to drive to and from a retinal laser appointment.
In the treatment of diabetic macular oedema with macular laser, the laser is applied in focal spots to areas of swollen retina to reduce the leakage of fluid into the retina with the aim of reducing further visual loss. The results of macular laser treatment are not immediate and initially the vision may get worse, before stabilizing. Several repeated laser treatments to the macula may be required to achieve the desired effect.
Often in the treatment of diabetic macular oedema, macular laser may not be effective, especially if the area of leakage is too close to the centre of the macula to actually treat with laser without risking damage to central vision from the laser. In these cases, the injection of a small quantity of an anti- Vascular Endothelial Growth Factor (Anti – VEGF) agent such as Avastin or corticosteroid into the eye may be necessary. Because the injection is delivered into the vitreous cavity of the eye, this injection is known as an intravitreal injection. Please refer to the section on intravitreal injections for further information regarding the procedure of intravitreal injection.
b) Anti-VEGF treatment for Diabetic Macular Oedema
Vascular endothelial growth factor (VEGF) is a growth factor produced by the eye which mediates the leakage of fluid into the retina and also the growth of abnormal blood vessels on the surface of the retina in diabetes. Drugs such as AVASTIN bind to VEGF thus inhibiting the effect of VEGF and have been shown to reduce the retinal swelling in diabetic macular oedema. Anti-VEGF treatment of diabetic macular oedema usually needs to be repeated on a regular basis. The interval between injections however may vary depending on the individual patient’s response to treatment.
c) Intraocular Corticosteroids for diabetic macular oedema
Intraocular corticosteroid injections also reduce retinal swelling in diabetic macular oedema and may require less frequent injections. However, repeated injections can lead to cataract formation and also cause glaucoma.
2) Treatment for Proliferative Diabetic Retinopathy
a) Pan Retinal Photocoagulation (PRP) for Proliferative Diabetic Retinopathy
When abnormal fragile new blood vessels with the potential to bleed begin to grow on the retinal surface in proliferative diabetic retinopathy (PDR), treatment with Pan Retinal Photocoagulation (PRP) needs to be commenced. In the early stages of proliferative diabetic retinopathy before the bleeding starts, the patient may be without any symptoms at all and therefore not realize that profound visual loss is imminent. During this procedure, the peripheral retina, which is not receiving adequate blood flow, is treated with laser, with the aim of inducing shrinkage of the abnormal blood vessels as well as stopping more abnormal blood vessels forming.
This treatment requires many laser spots, and thus may be divided into two or more separate sessions. PRP does not improve vision, but it can prevent the blinding complications of diabetic retinopathy such as bleeding into the vitreous cavity (vitreous haemorrhage) or tractional detachments of the retina. Side effects of PRP include some loss of peripheral and color vision and a decrease in night vision. Some patients experience blurry vision, which can be temporary or persist. Patients may also experience haemorrhage into the vitreous cavity despite the laser. It is very important to realize that regardless of these side effects, PRP has been shown to decrease the risk of vision loss in diabetic retinopathy.
b) Vitrectomy Surgery for Proliferative Diabetic Retinopathy
Although PRP is often successful in halting the process of proliferative diabetic retinopathy, laser treatment is ineffective in some cases. These patients may experience bleeding (vitreous hemorrhage), which makes it impossible for more laser to be delivered to the retina, or they may develop vitreous haemorrhage before any laser can even be applied. In some cases, this vitreous hemorrhage clears up on its own. However, if it does not clear up, a vitrectomy may be necessary. A vitrectomy may also be needed if the abnormal blood vessels progress to become scar tissue that pulls on the retina causing it to detach – tractional detachment of the retina.
A vitrectomy is the most common retinal surgical procedure performed. During a vitrectomy, the vitreous gel is removed from the vitreous cavity via key hole surgery. The reason for removing the vitreous in diabetic vitreous haemorrhage is because the abnormal blood vessels in proliferative diabetic retinopathy bleed into the vitreous cavity. This blood mixed with the vitreous obstructs and scatters light preventing it from being focused on the retina. The vitreous thus needs to be removed to allow light a clear path of focus onto the retina. The removed vitreous is replaced with saline solution which is infused through one of the key holes. Scar tissue that is pulling on the retina in the case of diabetic tractional retinal detachment can also be removed with fine dissection at the time of vitrectomy surgery.
Supplementary pan retinal photocoagulation can usually be applied at the time of diabetic vitrectomy surgery using a special laser probe if required. At the end of the procedure, a gas bubble may be used to splint the retina into place or in severe cases of tractional retinal detachment, a substance called silicone oil may be required.
Vitrectomy surgery is discussed in greater detail in the section entitled Vitrectomy Surgery