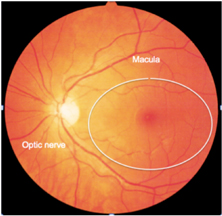
Age related macular degeneration (AMD) is a disease of advancing years. The macula is the centre of the light sensitive membrane at the back of the eye. This is the area that allows the visualisation of fine details, such as recognising faces or reading etc.
AMD is generally asymptomatic in its early stages and is only picked up by a routine sight check at the optometrist in many cases. The earliest findings are the appearance of yellow deposits (drusen) under the retina, which is the light sensitive membrane at the back of the eye.
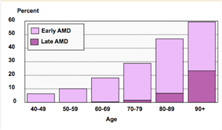
With advancing age, these deposits can lead to damage of the light sensitive cells of the macula, with subsequent visual deterioration (25% of people have vision impairment as a result of AMD by the age of 90 years).
AMD is a multifactorial disease, that is to say it has many causes. Ageing is the primary risk factor, although the genes that you inherit from your parents, certainly play a role. Additionally, lifestyle is also a modifiable risk factor, with smoking being associated with a quadrupling of the chance of AMD development. Several other putative factors have been identified over the last few years, such as high fat intake and obesity, alcohol, sedentary lifestyles as well as sun exposure. A protective role has also been hypothesized for those with high levels of oily fish and long chain polyunsaturated fatty acid intake and antioxidants.
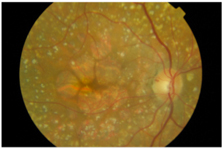
There are two types of AMD, the “dry” type and the “wet” type. The “dry” form of the disease occurs due to gradual loss of the light sensitive visual cells and up until recently was thought to be untreatable.
Areas of loss of the light sensitive cells, as well as drusen= DRY AMD
The mainstay of treatment for this form of the disease, is to advise against smoking and to increase intake of fruit and vegetables, which are rich in anti-oxidants, which are thought to protect the retina. The use of vitamin supplements in individuals with good diets is uncertain, with mixed results as to whether there is any additional benefit over and beyond lifestyle measures. Recently there has been interest in other potential forms of treatment for “dry” AMD. Unfortunately these treatments are still in their infancy and certainly experimental, with only laboratory work or only small scale studies on patients being done to date. Despite this there is a degree of excitement in the ophthalmic community about treatments such as laser to the drusen, to see if they can be removed prior to causing damage to the retina.
Another treatment being explored is the injection of substances into the eye called “growth factors” or “enzymes” which may delay the loss of retinal cells.
Wet AMD
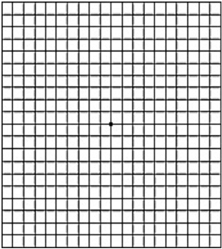
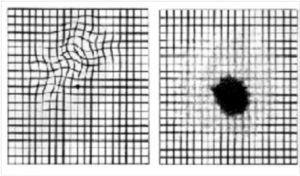
“Wet” AMD accounts for about 10% of cases of vision loss in macular degeneration. Wet AMD causes a sudden loss of vision, associated with distortion in many cases. This is often noticed as straight edges on door frames or windows being ‘wobbly’. Alternatively, when reading, the words may appear to go ‘up and down’. In some cases however, the distortion is not noticeable if the disease is only present in one eye. In this scenario, the better eye compensates for the affected eye and the AMD may only be discovered by chance at a routine optometrist check or if the better eye is covered by accident. An amsler chart may be useful to pick up early distortion.
AMSLER CHART
This test involves looking at the central black spot with one eye covered (whilst wearing reading glasses) to see if there are any areas that are distorted or missing.
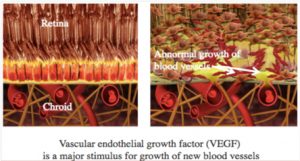
Wet AMD is a result of the growth of abnormal blood vessels from the layer under the retina (known as the choroid) in to the subretinal space.
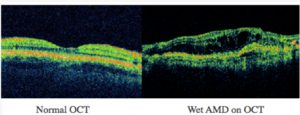
The blood vessels may bleed and leak fluid in to the retina (photographic film of the eye). This leakage may cause the retina to “swell”, leading to blurred vision, which progressively worsens. This swelling may be detected on an instrument called an OCT (optical coherence tomograph).
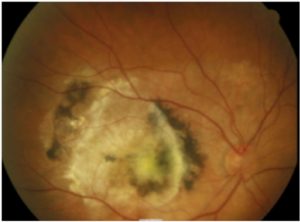
Without treatment, eventually, the healing responses in the eye shut down the blood vessels leading to a scar at the centre of the vision. This leads to irreversible vision loss in most individuals and may lead to “legal blindness” where the vision is poor centrally but reasonable around the outside.
Scar formation in the macula
Medical treatment for wet AMD
Fortunately treatment is available for wet AMD, although it involves a series of injections of drugs into the eye, to stabilise the blood vessels. Once stabilised, the blood and fluid are reabsorbed, preventing further vision loss and scar formation. The injections are given frequently at the start, but once the blood vessels are stabilised, less frequent injections may be required to maintain vision. The injection frequency is generally determined by monitoring of fluid build up via OCT scanning.
All injections are given under local anaesthetic and so discomfort is minimal, although the eye may be irritable on the day of the injection and may be red for a few days afterwards.
The two drugs commonly used in the treatment of wet AMD are Lucentis® (Ranibizumab) and Eylea® (Aflibercept). Both treatments have a very good chance of stabilising vision, although significant vision improvement only occurs in around one third of patients. Injections are likely to be on-going, as these drugs generally only stabilise the abnormal blood vessels, rather than eliminate them. Thus, without maintenance treatment, there is a fair chance that the blood vessels with reactivate, causing further damage.
In terms of optimising visual outcome following treatment, the key is early treatment (from first symptoms to first injection) and adequate treatment, with monthly injections being needed in some cases. Cessation of smoking is advisable, although not definitively proven to improve outcomes. With respect to medications, blood thinning agents such as asprin, warfarin and pradaxa may increase the risk of bleeding in wet AMD. Although ceasing these agents would be optimal, in most patients this is NOT possible, since this may compromise overall health. It is important to consult a general practioner or cardiologist, to discuss the overall benefits/ risks of these medications if you have wet AMD.